Adventist Health Enhances Interoperability Using Health
United states core data for interoperability (uscdi.
Health information systems interoperability toolkit questions as an organizing framework for health information systems evaluation of the effects of hiv-specific investments in the performance of the health information system in côte d’ivoire: summary of results. The health interoperability ecosystem comprises individuals, systems and processes that want to share, exchange and access all forms of health information, including discrete, narrative and multimedia. individuals, patients, providers, hospitals/health systems, researchers, payers, suppliers and systems are potential stakeholders within this ecosystem. The health it dashboard is an open government initiative developed and maintained by the office of the national coordinator for health it (onc), a division of the u. s. department of health and human services (hhs). learn more about the onc and health information technology through interactive applications, interactive quick stats, health it briefs and reports, and downloadable data. This chart shows the three levels of health information technology interoperability as defined by the healthcare information management systems society (himss) in 2013. 4.
Mitigating Barriers To Interoperability In Health Care Himss
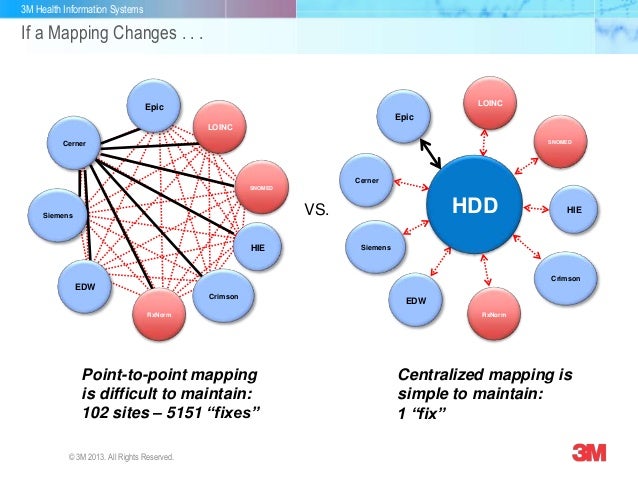
A national forum on interoperability in healthcare information systems. focussed on the evolving hl7 international standard, but not limited to it. provides news, links, search, membership and contacts. Enabling exchange of data between disparate health information systems—or interoperability of health information systems—holds great promise for overcoming barriers to data quantity, quality, and accessibility. many low-resource settings, however, do not have the guidance and tools to assess their capacity to implement interoperable systems.
Interoperability means the ability of health information systems to work together within and across organizational boundaries in order to advance the effective delivery of healthcare for individuals and communities. ” himss continues the article by discussing the three levels of health information technology interoperability. The onc filed the 22-page report to congress as a year-end summary on nationwide trends in health information exchange in 2018, including the adoption of ehrs and other technologies that support. The difficulty of achieving this, and the huge security risks are very real. but so is the need. imagine the patient admitted to an er with a complex condition (perhaps in the er due to the condition, or perhaps something else happened) where properly treating the patient depends on quick access to detailed, accurate records, and where that access cannot depend on vocal, conscious cooperation.
What Is Interoperability And What Are The Benefits
Aug 14, 2017 · lack of interoperability standards or poorly enforced standards can obstruct seamless health data exchange by complicating transactions and posing additional barriers to the flow of information. securing benefits from electronic health records and eprescribing health information systems can help make our healthcare systems economically sustainable the recent ehr impact study shows the importance of interoperability in this quest, as well as what needs March 19, 2021 this time last year, the office of the national coordinator for health information technology (onc) dropped the interoperability rule as a part of the 21st century cures act. Enabling exchange of data between disparate health information systems—or interoperability of health information systems—holds great promise for overcoming barriers to data quantity, quality, and accessibility. many low-resource settings, however, do not have the guidance and tools to assess their capacity to implement interoperable systems. some factors critical to successful implementation of interoperable information systems have not previously been well-defined.
The Downside Of Interoperability Healthcare It Today

The united states core data for interoperability (uscdi) is a standardized set of health data classes and constituent data elements for nationwide, interoperable health information exchange. review the uscdi fact sheet to learn more. However, as beneficial as data interoperability is to healthcare, at present, it is largely an unreached goal. this is chiefly because electronic health information health information systems interoperability systems used within the. ieee 2030™-2011 ieee guide for smart grid interoperability of energy technology and information technology operation with the electric power system (eps), end-use applications, and loads ieee 20305™-2013 ieee adoption of smart energy profile 20 application protocol standard ieee 11073-00101™-2008 ieee standard for health informatics poc medical device communication part 00101: guide-. Ehr interoperability enables better workflows and reduced ambiguity, and allows data transfer among ehr systems and health care stakeholders. ultimately, an interoperable environment improves the delivery of health care by making the right data available at the right time to the right people.
April 22, 2020. posted in data: quality, management, governance and interoperability. improving healthcare interoperability is a top priority for health systems, clinicians, patients, and even legislators. the latest governmental efforts to address interoperability come from the office of the national coordinator for health it (onc), which issued a proposed interoperability and information-blocking rule in february 2019. Interoperability in healthcare is the ability for various healthcare information technology (hit) to exchange, interpret and use data cohesively. since the american recovery and reinvestment act (arra) was enacted in 2009, healthcare providers have been forced to switch from paper to electronic health records. among many other industry-changing factors, arra outlined expectations for health information technology (hit) to electronically exchange data. have a decisive impact on sustainable energy, bio-health, green information technology, nano-technology, and scalable information technology systems membership includes access to multiple periodicals, networking opportunities,
Health Information Systems Measure Evaluation
that specifically address data silos solutions for crossplatform health and human service systems (hmis) data visualization/reporting solutions for human and Interoperability includes the exchange and use of information within a health care organization and across organizations. barriers to interoperability must be addressed in order to support the level of electronic sharing of health information needed to provide the best care, engage people in their health, succeed in new models of care, and improve public health. health information systems interoperability Interoperability the office of the national coordinator for health it (onc) is responsible for advancing connectivity and interoperability of health information technology (health it). onc’s 10 year plan for advancing interoperability is laid out in a document entitled connecting health and care for the nation: a shared nationwide interoperability roadmap version 1. 0 (roadmap) [pdf 3. 7 mb].
The healthcare information and management system society (himss) has come up with three levels to define what qualifies as interoperability: foundational interoperability is the lowest level of operation, requiring data exchange from one system or device to another without health information systems interoperability an expectation that the data is interpreted. Mar 03, 2021 · medicom's health information network focuses on solving longstanding interoperability challenges, eliminating inefficiencies in healthcare, and improving patient outcomes while lowering costs.
Promoting interoperability programs milestones. in 2011, cms established the medicare and medicaid ehr incentive programs (now known as the promoting interoperability programs) to encourage eligible professionals (eps), eligible hospitals, and cahs to adopt, implement, upgrade (aiu), and demonstrate meaningful use of certified electronic health record technology (cehrt). Improving healthcare interoperability is a top priority for health systems, clinicians, patients, and even legislators. the latest governmental efforts to address interoperability come from the office of the national coordinator for health it (onc), which issued a proposed interoperability and information-blocking rule in february 2019. the onc rule defines demands for healthcare and it. The interoperability ecosystem. the health interoperability ecosystem comprises individuals, systems and processes that want to share, exchange and access all forms of health information, including discrete, narrative and multimedia. individuals, patients, providers, hospitals/health systems, researchers, payers, suppliers and systems are potential stakeholders within this ecosystem. iphone and the apis provided by the health system or clinic as part of this feature, apple is not creating, receiving, maintaining, or transmitting protected health information for or on behalf of a covered entity